I was fortunate to be invited as speaker for the SHIP online course for HIV treatment hub staff in Mindanao and NCR, to enlighten them about prevention of mother to child transmission of HIV infection. However, the COVID-19 prevented me from giving my lecture live so here is my contribution to the cases discussed, as these are scenarios we encounter often.
1. Correct and consistent condom use reduces the risk of HIV transmission, but the risk is not zero.
2. ARV adherence reduces the HIV viral load down to undetectable. If undetectable = untransmissible. This means the risk of transmitting HIV to the HIV negative partner is very very low, but still the risk is not zero.
3. The HIV negative partner can take PrEP or pre-exposure prophylaxis. He/she takes ARV to reduce the risk of HIV transmission.
In reality, the only expression of love that is 100% free of risk of HIV transmission is abstinence.
Still, with our ARVs effective in reducing the HIV viral load, it is possible for serodiscordant couples to have unprotected penetrative sexual intercourse without transmitting the infection to their partners.
If the couple wishes to get pregnant, it would be best to learn about the woman's fertile period using the symptothermal method (calendar method, basal body temperature and cervical mucus method combined). The couple should have unprotected penetrative sexual intercourse every other day during the woman's fertile period. This reduces the exposure of the HIV negative partner to risk of HIV transmission and allows for greater chances of getting pregnant.
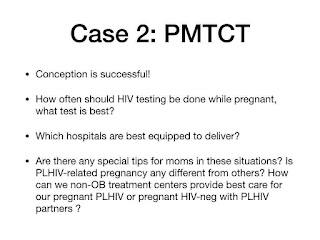
If the pregnant patient is PLHIV, no need to do HIV testing. We just request for baseline prenatal labs and screen for opportunistic infections. We request also for CD4 count and viral load. We usually deliver by cesarean section as this has been proven by research to significantly reduce risk of HIV transmission to the newborn. Any hospital capable of delivering a pregnant patient via cesarean section is equipped to deliver PLHIVs so long as standard precaution is observed to protect the healthcare worker. If we go back to the modes of transmission, then there is very little chance of the healthcare worker getting HIV via occupational transmission.
The PLHIV mother needs to weigh the benefits and risks of exclusive breastfeeding versus exclusive replacement feeding, but we do not recommend mixed feeding for the HIV-exposed newborn.
If the viral load near term is <1,000 then the patient may opt to deliver vaginally and even breastfeed with very low risk of HIV transmission to the newborn. The risk, however, is not zero.
For the HIV-negative pregnant partner of a PLHIV, HIV testing may be done as early as the first prenatal visit. HIV testing may be done every trimester if there is a continuing risk for HIV transmission. Otherwise, routine prenatal care should be provided for the pregnant patient and indications for cesarean delivery will follow the usual clinical practice guidelines.
As HIV treatment staff, we can help prenant PLHIVs by referring them as early as possible to OBGYNs for prenatal care so that complications can be identified early, ARVs can be initiated as early as 14 weeks and continued for life, those already on ARV can be assured that it is safe to continue taking their ARVs, to connect these PLHIV mothers to appropriate suport groups, as well as to celebrate their pregnancies not as problems to address but as gifts from God.
Life goes on with HIV, basta naka ARV!

No comments:
Post a Comment